The Ultimate Guide to Vaccine Storage
Understand Best Practices to Overcome Temperature and Storage Obstacles for Vaccines
Whether you’re administering or manufacturing vaccines, proper temperature control during vaccine storage is essential to preserve their integrity and achieve regulatory compliance.
Maintaining specific temperature ranges and overcoming storage obstacles are vital to safeguarding the potency and effectiveness of vaccines. By adhering to proper vaccine storage protocols, pharmaceutical companies and vaccination centers can ensure that vaccines remain safe and effective for administration to patients.
This guide will discuss best practices, challenges, regulations, and key considerations for pharmaceutical and logistics companies involved in the storage of life-saving vaccines.
What is Vaccine Storage?
Vaccine storage is the process of safely storing vaccines. Its primary concern is maintaining vaccines at proper temperatures to preserve their integrity. Regulatory compliant storage helps to ensure that vaccines can safely and effectively immunize patients when administered.
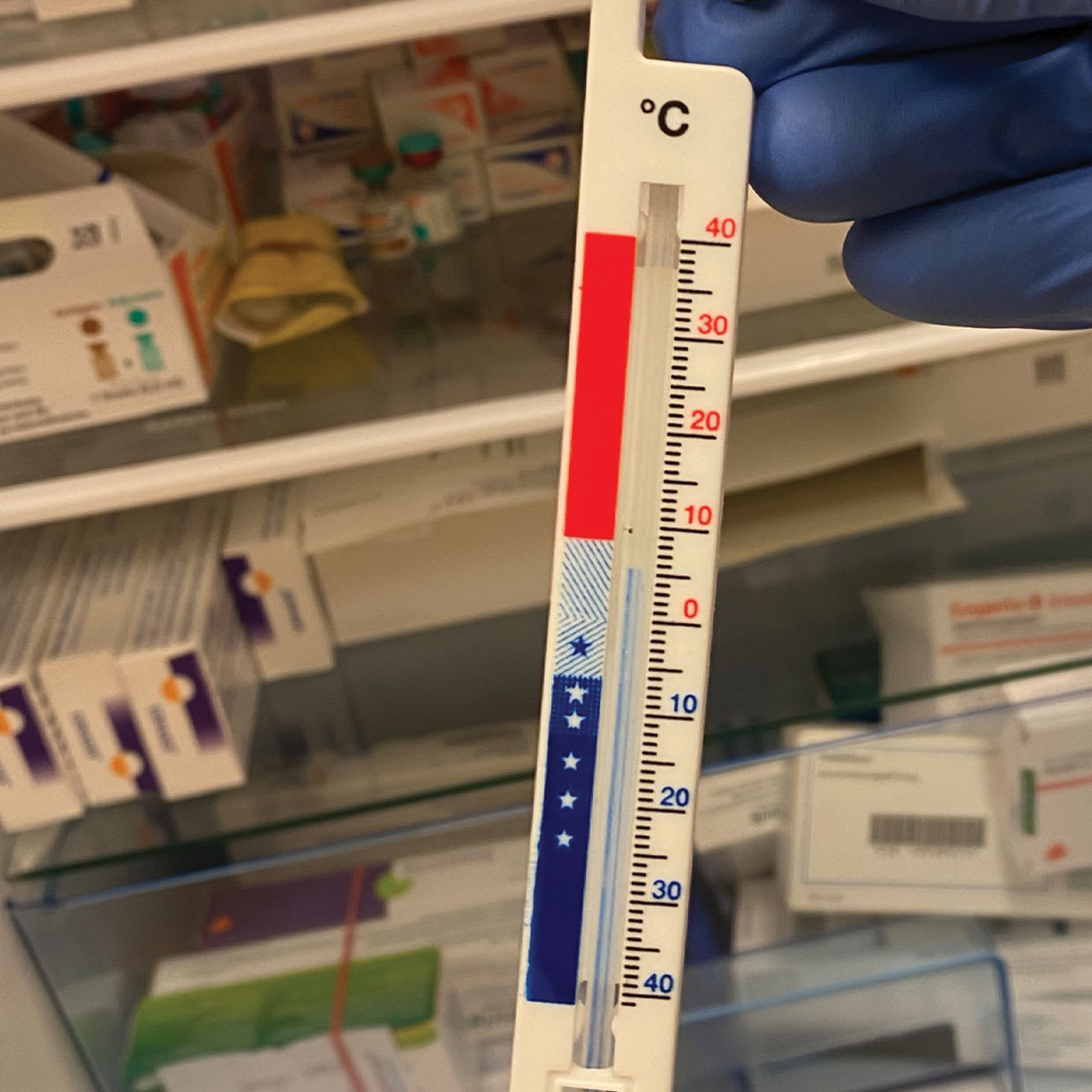
The majority of vaccines must be stored within a temperature range of +2°C to +8°C (+36°F to +46°F). This temperature range is commonly known as “refrigerated,” and care must be taken at the lower ends of the range since freezing temperatures can cause irreversible reactions in many vaccines. This is especially true for vaccines containing aluminum adjuvants.
Advisory and regulatory bodies like the U.S. Food & Drug Administration (FDA), Centers for Disease Control and Prevention (CDC), and World Health Organization (WHO) have devised vaccine storage standards which define the types of storage used, the procedures that should be followed, necessary temperature monitoring, and required documentation.
How to Store Vaccines
Although some vaccines have specific requirements for light exposure, the primary challenge in proper vaccine storage is ensuring each product is kept at the manufacturer’s label-stated temperature range, which prevents degradation and ensures vaccines remain efficacious.
Vaccines are often stored in refrigerators, freezers, or cold rooms, depending on their requirements. No matter how a vaccine is stored, the storage area must be accurately monitored to ensure that it is maintaining the proper temperature for the vaccines being stored. To achieve this, the CDC recommends using digital temperature monitoring devices specifically designed for pharmaceutical use.
Storing different types of vaccines may pose a challenge because individual products may have unique storage requirements, including specific temperature ranges. Here are best practices for storing some prevalent vaccines:
Prevnar 13 (Pneumonia Vaccine)
Prevnar 13, a pneumonia vaccine, should be stored at temperatures between +2°C and +8°C (+36°F and +46°F). It is especially important to avoid low excursions from this range, since the vaccine cannot be used if frozen and must be discarded.
Gardasil / Gardasil 9 (HPV vaccine)
Gardasil and Gardasil 9 should be stored at a temperature between +2°C and +8°C (+36°F and +46°F). Because it is a liquid vaccine containing an aluminum adjuvant, Gardasil and Gardasil 9 will permanently lose potency if exposed to freezing temperatures. For these types of vaccine, accurate temperature monitoring is crucial, as the vaccine must be discarded if it has been frozen.
COVID Vaccine
The COVID-19 vaccine, such as the Pfizer-BioNTech and Moderna vaccines, often requires ultra-cold storage. Pfizer-BioNTech's vaccine requires must be stored at a temperature between -80°C and -60°C (-112°F and -76°F). Moderna's vaccine, on the other hand, can be stored at a temperature of -25°C and -15°C (-13°F and +5°F). However, the newer Novavax COVID-19 vaccine can be stored between +2°C and +8°C and must not be frozen. It is critical to be aware of each COVID-19 vaccine’s recommended temperature for strict adherence during storage.
| Vaccine | Storage Temperature |
| COVID-19 (Johnson & Johnson) |
|
| COVID-19 (Moderna) |
|
| COVID-19 (Novavax) |
|
| COVID-19 (Pfizer-BioNTech) |
|
| Dengvaxia (Dengue Vaccine) |
|
| Diphtheria and tetanus vaccines (DT, Td) and their pertussis variations (DTaP, Tdap) |
|
| Gardasil / Gardasil 9 (HPV Vaccine) |
|
| Hepatitis A and Hepatitis B Vaccines |
|
| Influenza vaccines |
|
| M-M-R II (Measles, Mumps, Rubella Vaccine) |
|
| Meningococcal Vaccines |
|
| Ipol (Polio vaccine) |
|
| Prevnar 13 (Pneumonia Vaccine) |
|
| ProQuad (Measles, Mumps, Rubella, Varicella Vaccine) |
|
| RSV Vaccine (Abrysvo) |
|
| RSV Vaccine (Arexvy) |
|
| Rotarix (Monovalent Rotavirus Vaccine) |
|
| RotaTeq (Pentavalent Rotavirus Vaccine) |
|
| Shingrix (Shingles Vaccine) |
|
| Varivax (Varicella Vaccine) |
|
How Long Can Vaccines Be Stored?
When maintained at the manufacturer’s stated temperature range, a vaccine can be stored until the expiration date provided by its manufacturer. The exact duration will depend on the vaccine type. Storage conditions play a significant role in determining vaccine viability, especially for vaccines that need to be thawed or diluted.
Certain vaccines have strict requirements, and if they are removed from refrigeration and remain unadministered, they may need to be discarded. It is important to follow proper vaccine administration protocols and avoid unnecessary wastage by administering vaccines promptly and efficiently.
Challenges for Storing Vaccines

Because there are fewer variables, maintaining proper temperature control during storage is more predictable than during transportation. However, storing vaccines still presents various challenges that can impact their efficacy and safety. Some common obstacles include:
Temperature Fluctuations
Temperature fluctuations can make it difficult to ensure vaccines are continually stored within their recommended temperature range. Fluctuations can be caused by many factors, including outside temperatures, human behavior such as opening refrigerator doors, and the facility’s airflow. Monitoring and addressing any temperature fluctuations promptly can help mitigate risks. A thermal mapping study can identify regular temperature variations within a facility, and is a regulatory requirement for proper temperature management.
Lost Power
Power outages can cause refrigeration equipment to lose power, disrupting proper storage conditions. Having backup power sources, such as generators, and implementing contingency plans to maintain the required temperature range during power outages are essential for preserving vaccine efficacy. Plans for temporary power loss may include not opening refrigerators, or storing cold or frozen water bottles within the refrigerator to maintain cold temperatures until power resumes.
Temperature monitoring must continue during power outages, with any excursions and corrective actions fully documented, or vaccines may need to be discarded. With ColdStream® Site, battery backup and on-device storage ensure that power outages and disasters don’t interrupt monitoring. Each sensor stores a minimum of 17 days, and the local network controller keeps at least one year of temperature monitoring records. The complete data will synchronize with the cloud when connectivity is returned.
Best Practices for Storing Vaccines
There are a number of best practices for proper vaccine storage, which help to reduce the risk of compromised effectiveness. The CDC advises the following best practices, which storage facilities should consider implementing:
Check Temperature at the Start of Each Day
It is recommended to check and record the minimum and maximum refrigerator temperatures at the start of each workday to be aware of any temperature excursions or issues that may have occurred. If temperature monitoring equipment does not support recording minimum and maximum temperatures, the current temperature should be checked and recorded frequently.
Continuous real-time stationary temperature monitoring solutions like ColdStream Site automatically record the temperatures of all fridges and cold rooms equipped with sensors, eliminating the need for manual temperature checks and providing active alerts for any issues. Site-wide temperature check-ins can be conducted quickly from any location using a convenient cloud platform.
Create an Action Plan if Vaccine is Out of Range
Developing a robust action plan for temperature excursions ensures that necessary steps are taken to assess the affected vaccine's viability and determine appropriate follow up actions.
To handle temperature excursions effectively and avoid vaccine wastage, an action plan should include the following steps:
| Step | Action |
| Notify | Immediately report issues and label exposed vaccines as “do not use.” |
| Document | Document all details of the excursion, including date, time, and temperature. |
| Contact | Contact manufacturers or immunization program for guidance. |
| Correct | Address the issue, fixing faulty refrigeration equipment. |
Create a Plan for When Facilities Lose Power
A facility losing power presents a major threat to the quality of the vaccines being stored there, and it is important to develop a plan for these instances. This plan should include backup power sources or alternative storage sites, regular maintenance checks, and procedures for maintaining temperature control during power disruptions. The plan must be accessible to all staff.
Some guidelines to follow when creating a power outage response plan may include:
- Identifying a back-up site, or a back-up power source like a generator, where the vaccines will be stored in the event of a power outage
- Continuing to monitor temperatures, ideally using a solution designed to function reliably in the event of disruptions, such as ColdStream Site
- Keeping storage units, cold rooms, and refrigerators closed until power is restored (if the disruption is short-term)
- Utilizing coolant gel packs or frozen water bottles to maintain cold storage temperatures (if the disruption is short-term)
- Documenting the outage, especially any temperature excursions
- Reporting any losses to the Office of Immunization
Rotate Vaccines by Expiration Date
Rotating vaccine stock based on their expiration dates ensures that older vaccines are used first, reducing unnecessary wastage and minimizing the risk of administering expired vaccines.
Additionally, vaccine inventory should be limited to a 60-to-90 day supply for monthly vaccines and a two-to-four week supply for flu vaccines.
Conduct Temperature Mapping Studies to Identify Risk Areas
Temperature mapping studies involve analyzing temperature variations within storage facilities and refrigerators to better understand the overall temperature control of the vaccine storage area, and are a regulatory requirement for storing vaccines in many parts of the world. They should be conducted in both summer and winter seasons to account for seasonal temperature changes.
By identifying areas prone to temperature fluctuations, measures and processes can be implemented to ensure consistent storage conditions throughout the facility. This helps ensure vaccines are stored at their correct temperatures.
A thorough thermal mapping study, such as those conducted by Sensitech’s professional services team, may also identify temperature control challenges in a facility’s standard operating procedures, such as procedural issues when unloading trucks or accessing cold rooms.
Regulations for Vaccine Storage
Many regulations and guidelines affect vaccine storage practices. As well as country-specific regulations, anybody storing vaccines should be familiar with EU GDP guidelines, USP <1079>, USP <659>, the CDC’s Vaccine Storage and Handling Pink Book, and the WHO Guidelines on the International Packaging and Shipping of Vaccines.
These guidelines provide overarching principles for the proper storage and handling of vaccines, such as temperature control, inventory management, storage equipment requirements, and documentation procedures.
We will explore some common vaccine storage requirements below. Sensitech’s experts can provide more thorough guidance to help advise whether your vaccine storage program is regulatory compliant.
Temperature
Any area used for vaccine storage is required to maintain temperature within the range specified on each product’s label. Storage temperatures must be accurately monitored, and refrigeration units should be qualified (assessed to consistently maintain the required temperature) where possible.
Refrigerators should be set at 5°C (40°F) to maintain temperatures between 2°C and 8°C (36°F and 46°F), and the CDC’s vaccine storage best practices state that freezers used for vaccines should maintain temperatures between -50°C and -15°C (-58°F and +5°F) – note that this is different from typical pharmaceutical freezer temperatures of −25°C to −10°C. Care must be taken, however, since some vaccines may have temperature requirements outside these ranges.
Refrigeration Equipment
It is recommended to use purpose-built refrigeration units, since these are designed for biologics and provide better temperature control, better circulation for uniform temperature, and can recover correct temperatures more quickly. Household-grade refrigerators and freezers may be used where necessary, though they should be stand-alone units.
Vaccines must not be stored in a combined refrigerator-freezer with a single door, even for temporary storage, as these units pose a considerable risk of freezing vaccines.
Vaccines must be stored in their original packaging until ready for administration. This prevents light incursion, provides additional temperature stability, and reduces the risk of administration errors.
Temperature Monitoring Devices
Every vaccine storage unit must have a temperature monitoring device. The CDC recommends using digital continuous temperature monitoring solutions with Certificates of Calibration, programmable logging interval, alarms, and +/-0.5°C accuracy traceable to National Institute of Standards and Technology (NIST) standards.
Temperature monitoring equipment should be specifically designed for life sciences use, as consumer or food grade temperature monitoring devices do not meet the standards for calibration or accuracy required to ensure safe vaccine storage temperatures.
Equipment used for temperature monitoring during transport within vehicles and/or containers should be maintained and calibrated at regular intervals at least once a year. Sensitech’s ColdStream® Select provides this annual calibration as part of its service.
Data Storage
Digital data stored from temperature monitoring devices must meet regulatory requirements in order to be considered trustworthy, reliable, and equivalent to paper records. The two most notable such regulations are the FDA's 21 CFR part 11 and the EU’s GDP Annex 11, both of which require controls including system validations, audit trails, electronic signatures, and documentation. A validated stationary monitoring solution designed for life sciences, such as ColdStream Site, will meet these requirements.
Final Thoughts
Proper vaccine storage is a critical component of the pharmaceutical and logistics industries. By following best practices, adhering to regulations, and being proactive in addressing challenges, these stakeholders can ensure that vaccines remain effective and safe to administer to patients. Implementing robust storage protocols will contribute to maintaining the integrity of vaccines, ultimately protecting the health of individuals who receive them.
Our vaccine-ready stationary temperature monitoring solutions provide powerful, validated temperature monitoring for vaccine storage, with secure cloud-based data access and EU GDP Annex 11 / FDA 21 CFR Part 11 compliant data storage. For more information, Contact Us today.